Initial orthostatic hypotension as a cause of syncope in an adolescent
N. van Dijk, M.P. Harms, W. Wieling
Department of Medicine, Academic Medical Centre, University of Amsterdam, Amsterdam (The Netherlands)
A 17 year old man was referred for evaluation of complaints of light-headedness and muscle weakness shortly (5-10 sec) after standing up or when standing still after physical exercise. He had fainted on numerous occasions just after standing up. The complaints existed already for 8 years. He had visited 5 different medical specialists and was referred for psychiatric evaluation, but no diagnosis had been made.
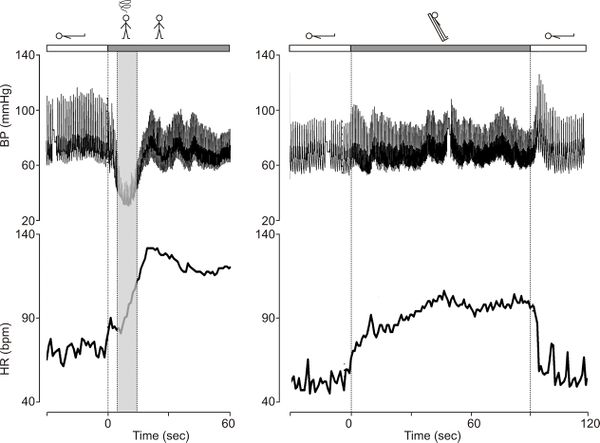
The patient was tall (197 cm) and slender (73 kg). He was examined using a Finapres model 5 (TNO Biomedical Instrumentation, Amsterdam, The Netherlands), which measures rapid changes in blood pressure continuously, accurately and non-invasively[1]. In supine position finger arterial pressure was 105/60 mmHg with a heart rate of 70 bpm. The initial drop in blood pressure (Fig 1. left panel) upon active standing was abnormally large (-65 mmHg systolic and -30 mmHg diastolic; normally blood pressure does not drop for more than -40 mmHg systolic and -20 mmHg diastolic). During the drop in blood pressure the patient had recognizable symptoms. His complaints disappeared within 20 seconds after standing up. After 1 and 5 minutes the patient’s blood pressure were 80/55 mmHg and 100/65 respectively and his heart rate was 120 bpm. During head-up tilt there was no drop in blood pressure and the patient expressed no symptoms (Fig. 1, right panel).
The patient was diagnosed with initial orthostatic hypotension. He was relieved that an explanation for his symptoms was finally established. The patient was advised to raise his water and salt intake and was prescribed a mineralocorticoid (fludrocortisone 0,1 mg/day). Furthermore he was advised to use lower body muscle tensing as a preventive measure in case of symptoms (see Casus 3 in this section). Over the years his complaints have diminished significantly.
Editor's comments
Syncope or particularly pre-syncope upon standing is observed much more commonly in the young than in adults. Almost all teenagers and adolescents are familiar with a brief feeling of lightheadedness and some visual blurring within a few seconds of standing up quickly. Symptoms typically resolve spontaneously within 20 seconds. Such complaints are most common after prolonged supine rest or after arising from the squatted position (see Casus 2 and 3 in this section)[2][1][3]. The complaints are caused by a transient fall in arterial pressure which occurs upon active standing. This transient fall in blood pressure during active standing is a physiological response[4]. However, normally blood pressure does not drop for more than -40 mmHg systolic and -20 mmHg diastolic[1].This initial drop in blood pressure is less dramatic or not at all present upon a passive head-up tilt. In some instances the symptoms are severe and true syncope may occur upon standing in otherwise healthy subjects. A recent study in 394 medical students showed that in 8% standing up was the trigger for transient loss of consciousness[5].
The initial transient fall in pressure in normal young subjects is caused by vasodilatation in active muscles during standing up[4]. Patients with the most severe complaints tend to be tall with an asthenic habitus and poorly developed musculature[6]. Often the patients also have a postural tachycardia and a tendency to faint during prolonged standing[7][8]. For the diagnosis of initial orthostatic hypotension history taking is the most important tool. The onset of symptoms between 5-10 s and disappearance within 20 seconds is typical for this clinical condition. The diagnosis can only be confirmed by an active standing test with continuous blood pressure monitoring using a Finapres device. A positive test (symptoms and an abnormally large initial fall in finger bloodpressure) is a very specific, but in our experience not a sensitive test. Because initial orthostatic hypotension is associated with active arising, tilt testing (i.e. head up tilting) is not the provoking test and not indicated.
Treatment of initial orthostatic hypotension is symptomatic. Goal is to diminish the drop in blood pressure during standing up. A clear explanation of the underlying mechanism and avoidance of the main triggers (rapid raise) are the main treatment-options. A novel approach is training in blood pressure rising manoeuvres. We have found lower body muscle tensing immediately after standing up very effective to decrease the fall in pressure[9].(see also Casus 3 in this section). In addition volume-expansion can be applied by raising water- and salt-intake[10]. In severe cases head-up sleeping or pharmacological treatment with mineralocorticoids (fludrocortisone) can be considered (see Casus 7 in this section].
References
-
Wieling W, Karemaker JM. Non-invasive continuous recording of heart rate and blood pressure in the evaluation of neurovascular control. In: Bannister R, Mathias CJ, eds. Autonomic failure: a textbook of clinical disorders of the autonomic nervous system. 4th ed. New York: University Press; 1999:197-210.
-
Parts of this case were published earlier:: van Dijk N, Harms MP, Wieling W. Three patients with unrecognized orthostatic intolerance. Ned Tijdschr Geneeskd 2000;144:249-254. We thank the Nederlands Tijdschrift voor Geneeskunde for permitting this reproduction.
- Wieling W, Ganzeboom KS, and Saul JP. Reflex syncope in children and adolescents. Heart. 2004 Sep;90(9):1094-100. DOI:10.1136/hrt.2003.022996 |
- Sprangers RL, Wesseling KH, Imholz AL, Imholz BP, and Wieling W. Initial blood pressure fall on stand up and exercise explained by changes in total peripheral resistance. J Appl Physiol (1985). 1991 Feb;70(2):523-30. DOI:10.1152/jappl.1991.70.2.523 |
- Ganzeboom KS, Colman N, Reitsma JB, Shen WK, and Wieling W. Prevalence and triggers of syncope in medical students. Am J Cardiol. 2003 Apr 15;91(8):1006-8, A8. DOI:10.1016/s0002-9149(03)00127-9 |
- van Dijk N, Immink RV, Mulder BJ, van Lieshout JJ, and Wieling W. Orthostatic blood pressure control in Marfan's syndrome. Europace. 2005 Jan;7(1):25-7. DOI:10.1016/j.eupc.2004.05.009 |
- Dambrink JH, Imholz BP, Karemaker JM, and Wieling W. Postural dizziness and transient hypotension in two healthy teenagers. Clin Auton Res. 1991 Dec;1(4):281-7. DOI:10.1007/BF01819833 |
- Tanaka H, Yamaguchi H, Matushima R, and Tamai H. Instantaneous orthostatic hypotension in children and adolescents: a new entity of orthostatic intolerance. Pediatr Res. 1999 Dec;46(6):691-6. DOI:10.1203/00006450-199912000-00022 |
-
Krediet CT, Wieling W. Physical counter are effective in diminishing initial orthostatic hypotension. Clin Auton Res 2004;14:311-312.
- Shichiri M, Tanaka H, Takaya R, and Tamai H. Efficacy of high sodium intake in a boy with instantaneous orthostatic hypotension. Clin Auton Res. 2002 Feb;12(1):47-50. DOI:10.1007/s102860200010 |