Vasovagal fainting in children and teenagers: Difference between revisions
No edit summary |
No edit summary |
||
| (5 intermediate revisions by 2 users not shown) | |||
| Line 11: | Line 11: | ||
== Editor's comments == | == Editor's comments == | ||
By far the most common cause of transient loss of consciousness in young subjects is a reflex syncopal event and in particular a vasovagal faint | By far the most common cause of transient loss of consciousness in young subjects is a reflex syncopal event and in particular a vasovagal faint <cite>Wieling</cite>,<cite>Stephenson</cite>. A variety of triggers have been identified [Table 1]. | ||
{| class="wikitable" border="0" style="width: 55%" | {| class="wikitable" border="0" style="width: 55%" | ||
| Line 60: | Line 60: | ||
Two clinical scenarios in particular are known to provoke vasovagal faints in young subjects. First and foremost are the situations that increase pooling of venous blood below the heart, such as long periods of standing motionless, particularly in combination with elevated ambient temperatures. | Two clinical scenarios in particular are known to provoke vasovagal faints in young subjects. First and foremost are the situations that increase pooling of venous blood below the heart, such as long periods of standing motionless, particularly in combination with elevated ambient temperatures. | ||
Young subjects often experience prodromal signs and symptoms when a spontaneous vasovagal syncope is imminent (Table 2) | Young subjects often experience prodromal signs and symptoms when a spontaneous vasovagal syncope is imminent (Table 2) <cite>Wieling</cite>,<cite>Stephenson</cite>. | ||
{{case_present| | {{case_present| | ||
These prodromes are reported to be more intense than those in elderly subjects, perhaps related to more robust autonomic control. However, some young subjects have little or no prodromal symptoms or do not recognize them as in our patient during the first episode. Their collapse occurs without warning. The second scenario is syncope at the time of distressing emotional situations or pain, which appears also to be more common in the young. A typical example is an event during blood drawing . Other emotional triggers reported in young subjects include having the hair cut or brushed (as in our young patient), eye examinations or manipulation, dental procedures or watching televison programs about medical matters or animal biology | These prodromes are reported to be more intense than those in elderly subjects, perhaps related to more robust autonomic control. However, some young subjects have little or no prodromal symptoms or do not recognize them as in our patient during the first episode. Their collapse occurs without warning. The second scenario is syncope at the time of distressing emotional situations or pain, which appears also to be more common in the young. A typical example is an event during blood drawing . Other emotional triggers reported in young subjects include having the hair cut or brushed (as in our young patient), eye examinations or manipulation, dental procedures or watching televison programs about medical matters or animal biology <cite>Wieling</cite>,<cite>Stephenson</cite><cite>Lewis</cite><cite>Hall</cite>. | ||
The clinical presentation of vasovagal syncope may vary widely both within and among young patients | The clinical presentation of vasovagal syncope may vary widely both within and among young patients <cite>Wieling</cite>,<cite>Stephenson</cite>. The trigger may be emotional for one event, and postural for another. Further, vasovagal episodes may occur without an identifiable trigger, even in patients who are sitting. Apparently benign vasovagal episodes may also occur during normal daily exercises like playing, walking or cycling and even during strenuous exercise. However, in case of syncope during exercise a cardiac cause like a long QT syndrome should always be excluded <cite>Wieling</cite>,<cite>Stephenson</cite>. | ||
It is important to consider all episodes and not just one unexplained event. In case of a history of a typical vasovagal syncope for some of the episodes, the atypical presentations are very likely to be of vasovagal origin as well | It is important to consider all episodes and not just one unexplained event. In case of a history of a typical vasovagal syncope for some of the episodes, the atypical presentations are very likely to be of vasovagal origin as well <cite>Wieling</cite>,<cite>Stephenson</cite>. However, events that occur while supine in the absence of an emotional stimulus are unlikely to be vasovagal. Neverthelesss, vasovagal syncope during sleep has been described <cite>Krediet</cite>. Additional reflex syncopal events that are typical for young subjects include initital orthostatic hypotension (see casus 1 in section orthostatic hypotension), adolescent stretch syncope <cite>Pelekanos</cite>, postural tachycardia syndrome and the fainting lark (see casus 4 in section orthostatic hypotension. ‘Stretch' syncope may occur during stretching with the neck hyperextended while standing. It is reported to occur in teenage boys with a familial tendency to faint. It has been attributed to effects of straining (which decreases systemic blood pressure) in combination with decreased cerebral blood flow caused by mechanical compression of the vertebral arteries <cite>Pelekanos</cite>. | ||
The incidence of syncope coming to medical attention appears to be clearly increased in two age groups i.e. in the young and in the old (Figure 1) | The incidence of syncope coming to medical attention appears to be clearly increased in two age groups i.e. in the young and in the old (Figure 1) <cite>Wieling</cite><cite>Colman</cite>. | ||
}} | }} | ||
[[File:Figure1. | [[File:Figure1.svg | 500px|thumb|left|Frequency of the complaint fainting as reason for encounter in general practice in the Netherlands. Data are obtained from the general practitioners transition project. It concerns an analysis of 93.297 patient years. The arrow around 1 year is to indicate that a small peak occurs between 6-18 months (breath-holding spells). <cite>Colman</cite>]] | ||
{{case_present| | {{case_present| | ||
An incidence peak occurs around the age of 15 years, with females having more than twice the incidence of males | An incidence peak occurs around the age of 15 years, with females having more than twice the incidence of males <cite>Ganzeboom</cite>. | ||
Syncope is an infrequent occurrence in adults. The incidence of syncope progressively increases over the age of about 40 years to become high at in the older age groups. A lower peak occurs in older infants and toddlers, most commonly referred to as “breath-holding spells” | Syncope is an infrequent occurrence in adults. The incidence of syncope progressively increases over the age of about 40 years to become high at in the older age groups. A lower peak occurs in older infants and toddlers, most commonly referred to as “breath-holding spells” | ||
The incidence of syncope in young subjects coming to medical attention varies from approximately 0.5 to 3 cases per 1000 (0.05 – 0.3%) | The incidence of syncope in young subjects coming to medical attention varies from approximately 0.5 to 3 cases per 1000 (0.05 – 0.3%) <cite>Driscoll</cite>. Syncopal events which do not reach medical attention occur much more frequently. In fact, the recently published results of a survey of students averaging 20 years of age demonstrated that about 20% of male and 50% of females report to have experienced at least one syncopal episode <cite>Ganzeboom</cite>. By comparison, the prevalence of epileptic seizures in a similar age group is about 5 per 1000 (0.5%) <cite>Wallace</cite> and cardiac syncope (i.e., cardiac arrhythmias or structural heart disease) is even far less common <cite>Wieling</cite><cite>Colman</cite>. | ||
}} | }} | ||
{{clr}} | |||
== References == | == References == | ||
<biblio> | <biblio> | ||
# | #Wieling pmid=15310717 | ||
#Stephenson Stephenson JBP, McLeod KA. Reflex anoxic seizures. In: Recent advances in Pediatrics 18. David TJ ed. Churchill Livingstone, Edinburgh 2000 | |||
#Lewis pmid=8464678 | |||
#Hall pmid=678863 | |||
#Krediet pmid=15084573 | |||
#Pelekanos pmid=2320248 | |||
#Colman pmid=15480937 | |||
#Ganzeboom pmid=12686351 | |||
#Driscoll pmid=9120157 | |||
#Wallace pmid=9872246 | |||
</biblio> | </biblio> | ||
Latest revision as of 15:21, 7 July 2014
W. Wieling
Department of Internal Medicine, Academic Medical Center, University of Amsterdam, (The Netherlands)
A 14 year old boy was referred to our syncope unit for analysis of an unexplained episode of transient loss of consciousness. The episode occurred while standing still during a soccer competition game after a run. The patient denied prodromal symptoms. The duration of the loss of consciousness was short (< 1 min).
The general health of the patient was excellent. Evaluations by two pediatricians, a pediatric cardiologist and a pediatric neurologist including several EKG, an echocardiogram, a 24 hours Holter, an exercise test and blood examinations were unremarkable. He was advised to restrain from playing soccer.
Additional history taking revealed that three addditional episodes of transient loss of consciousness had occurred. One while standing still on a warm day during a vacation with his parents in Paris while a street artist was making a drawing of him. The other episodes occurred also standing motionless while a girlfriend of his mother was giving him a haircut. During this episodes he was reported to be pale and sweating. Nausea was present during one of the episodes. Based on the historical findings reflex vasovagal syncope was diagnosed. The mechanism underlying the episodes were explained to the patient and his parents. The young patient and his parents were reassured and informed about life style measures. He started to play soccer again. No more syncopal episodes occurred.
Editor's comments
By far the most common cause of transient loss of consciousness in young subjects is a reflex syncopal event and in particular a vasovagal faint [1],[2]. A variety of triggers have been identified [Table 1].
| Table 1. Classification of syncope based on triggers | |
|---|---|
| A) Reflex mediated Vasovagal syncope | B) Mechanical/hydraulic factors |
Vasovagal syncope
Ocular syncope
Urogenital
|
Initial orthostatic hypotension
Increased intrathoracic pressure: cough and sneeeze syncope
|
| Table 2:Typical Premonitory Symptoms for Reflex Syncope |
|---|
|
Two clinical scenarios in particular are known to provoke vasovagal faints in young subjects. First and foremost are the situations that increase pooling of venous blood below the heart, such as long periods of standing motionless, particularly in combination with elevated ambient temperatures. Young subjects often experience prodromal signs and symptoms when a spontaneous vasovagal syncope is imminent (Table 2) [1],[2].
These prodromes are reported to be more intense than those in elderly subjects, perhaps related to more robust autonomic control. However, some young subjects have little or no prodromal symptoms or do not recognize them as in our patient during the first episode. Their collapse occurs without warning. The second scenario is syncope at the time of distressing emotional situations or pain, which appears also to be more common in the young. A typical example is an event during blood drawing . Other emotional triggers reported in young subjects include having the hair cut or brushed (as in our young patient), eye examinations or manipulation, dental procedures or watching televison programs about medical matters or animal biology [1],[2][3][4].
The clinical presentation of vasovagal syncope may vary widely both within and among young patients [1],[2]. The trigger may be emotional for one event, and postural for another. Further, vasovagal episodes may occur without an identifiable trigger, even in patients who are sitting. Apparently benign vasovagal episodes may also occur during normal daily exercises like playing, walking or cycling and even during strenuous exercise. However, in case of syncope during exercise a cardiac cause like a long QT syndrome should always be excluded [1],[2].
It is important to consider all episodes and not just one unexplained event. In case of a history of a typical vasovagal syncope for some of the episodes, the atypical presentations are very likely to be of vasovagal origin as well [1],[2]. However, events that occur while supine in the absence of an emotional stimulus are unlikely to be vasovagal. Neverthelesss, vasovagal syncope during sleep has been described [5]. Additional reflex syncopal events that are typical for young subjects include initital orthostatic hypotension (see casus 1 in section orthostatic hypotension), adolescent stretch syncope [6], postural tachycardia syndrome and the fainting lark (see casus 4 in section orthostatic hypotension. ‘Stretch' syncope may occur during stretching with the neck hyperextended while standing. It is reported to occur in teenage boys with a familial tendency to faint. It has been attributed to effects of straining (which decreases systemic blood pressure) in combination with decreased cerebral blood flow caused by mechanical compression of the vertebral arteries [6].
The incidence of syncope coming to medical attention appears to be clearly increased in two age groups i.e. in the young and in the old (Figure 1) [1][7].
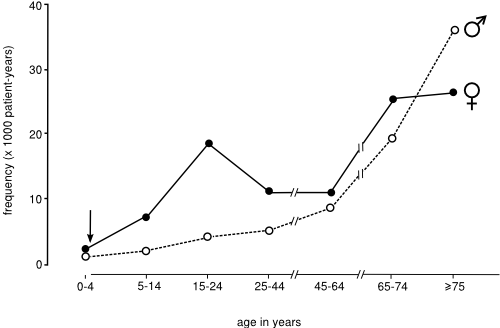
An incidence peak occurs around the age of 15 years, with females having more than twice the incidence of males [8]. Syncope is an infrequent occurrence in adults. The incidence of syncope progressively increases over the age of about 40 years to become high at in the older age groups. A lower peak occurs in older infants and toddlers, most commonly referred to as “breath-holding spells”
The incidence of syncope in young subjects coming to medical attention varies from approximately 0.5 to 3 cases per 1000 (0.05 – 0.3%) [9]. Syncopal events which do not reach medical attention occur much more frequently. In fact, the recently published results of a survey of students averaging 20 years of age demonstrated that about 20% of male and 50% of females report to have experienced at least one syncopal episode [8]. By comparison, the prevalence of epileptic seizures in a similar age group is about 5 per 1000 (0.5%) [10] and cardiac syncope (i.e., cardiac arrhythmias or structural heart disease) is even far less common [1][7].
References
- Wieling W, Ganzeboom KS, and Saul JP. Reflex syncope in children and adolescents. Heart. 2004 Sep;90(9):1094-100. DOI:10.1136/hrt.2003.022996 |
-
Stephenson JBP, McLeod KA. Reflex anoxic seizures. In: Recent advances in Pediatrics 18. David TJ ed. Churchill Livingstone, Edinburgh 2000
- Lewis DW and Frank LM. Hair-grooming syncope seizures. Pediatrics. 1993 Apr;91(4):836-8.
- Hall DM. Non-epileptic television syncope. Br Med J. 1978 Jul 15;2(6131):205. DOI:10.1136/bmj.2.6131.205 |
- Krediet CT, Jardine DL, Cortelli P, Visman AG, and Wieling W. Vasovagal syncope interrupting sleep?. Heart. 2004 May;90(5):e25. DOI:10.1136/hrt.2003.031294 |
- Pelekanos JT, Dooley JM, Camfield PR, and Finley J. Stretch syncope in adolescence. Neurology. 1990 Apr;40(4):705-7. DOI:10.1212/wnl.40.4.705 |
- Colman N, Nahm K, Ganzeboom KS, Shen WK, Reitsma J, Linzer M, Wieling W, and Kaufmann H. Epidemiology of reflex syncope. Clin Auton Res. 2004 Oct;14 Suppl 1:9-17. DOI:10.1007/s10286-004-1003-3 |
- Ganzeboom KS, Colman N, Reitsma JB, Shen WK, and Wieling W. Prevalence and triggers of syncope in medical students. Am J Cardiol. 2003 Apr 15;91(8):1006-8, A8. DOI:10.1016/s0002-9149(03)00127-9 |
- Driscoll DJ, Jacobsen SJ, Porter CJ, and Wollan PC. Syncope in children and adolescents. J Am Coll Cardiol. 1997 Apr;29(5):1039-45. DOI:10.1016/s0735-1097(97)00020-x |
- Wallace H, Shorvon S, and Tallis R. Age-specific incidence and prevalence rates of treated epilepsy in an unselected population of 2,052,922 and age-specific fertility rates of women with epilepsy. Lancet. 1998 Dec 19-26;352(9145):1970-3. DOI:10.1016/S0140-6736(98)04512-7 |