Physical manoeuvres that reduce postural hypotension in autonomic failure
W. Wieling, J.J. van Lieshout, A.M. van Leeuwen
Department of Medicine, Academic Medical Centre, University of Amsterdam, Amsterdam (The Netherlands)
We describe a young female patient who was healthy until she presented with severe disabling orthostatic hypotension shortly after lymph node cancer, Hodgkin’s disease was diagnosed at an age of 22 years[1]. She even fainted when attempting to sit upright and was only able to move around sitting in a wheelchair with her knees drawn up. She also had a dry mouth, couldn’t perspire and found it hard to read. In addition, she had constipation with bouts of diarrhea and couldn’t pass urine easily.
Acute pandysautonomia, a generalized disorder of the autonomic nervous system, was diagnosed with the features of a hypoadrenergic orthostatic hypotension syndrome. In the cardio-vascular system she had an isolated sympathetic postganglionic lesion but, despite other features of parasympathetic impairment, had intact parasympathetic control of heart rate[2][3].
Treatment with chemotherapy and radiation resulted in complete remission of Hodgkin’s disease. Her saliva production, bowel movements and urinary bladder function returned to normal. Severe orthostatic hypotension however persisted, despite treatment with fludrocortisone 200 mcg daily. Warning symptoms of a very low blood pressure consisted of lightheadedness, visual disturbances, ringing in the ears, yawning and pain in the neck.
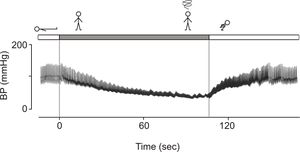
During this period, she discovered a series of manoeuvres which helped to reduce the symptoms of orthostatic hypotension. The light-headedness, which developed soon after arising from the supine position, was relieved by squatting (Fig. 1).
Orthostatic tolerance improved distinctly when standing with the head bent and with contracted abdominal muscles. By applying these techniques she was able to walk short distances at home. When shopping and needing an item out of reach she arose from her wheelchair, lifted her arms quickly to pick up the item from the shelves and squatted immediately thereafter, thereby preventing syncope. Climbing stairs was impossible and she reached her apartment on the first floor by hopping backwards up the stairs. Interestingly, she observed that in a swimming pool, if the water was on the level of her belly button, she could walk unlimited. This beneficial effect can be attributed to the hydrostatic counter-pressure effect of water.
One year after the onset of symptoms of orthostatic hypotension she was admitted to further improve therapy. The hypoadrenergic orthostatic hypotension syndrome was still present. She was able to stand still in upright position for about 1 minute only. However, her orthostatic tolerance improved distinctly upon chronic expansion of plasma volume. She was discharged, walking upright, with a regimen of fludrocortisone (300 mcg), sodium chloride (around 12 g). She had learned to sleep with the bed in a 12° head-up tilted position (about 12 inches elevation). This has been described in detail[4].
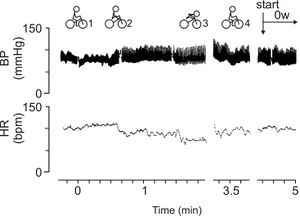
After discharge she reported that she felt reasonably well and was not seriously restrained in daily life duties. At that time she started a laborious part-time job as a social worker in an institution for battered women. She regularly went for bicycle rides, initially with her friend as the rear rider on a tandem covering distances of up to 60 km a day, but in due course on her own as well. This faced her with a new problem: light-headedness during and immediately following cycling. She prevented fainting by short intermittent resting periods with her knees pulled-up on the frame. A further difficulty was to stop at red traffic-lights as stopping cycling almost instantaneously caused dizziness; she discovered that by bending over de handle bar of her bicycle prevented fainting. On investigation of her ‘bicycle manoeuvres’ in the laboratory (Fig. 2, positions 1 to 4), her blood pressure fell progressively when she was sitting motionless on the bicycle. By pulling up her legs blood pressure increased; bending over the handle bar resulted in an additional increase in pulse pressure. On returning her feet from the frame to the pedals blood pressure again dropped.
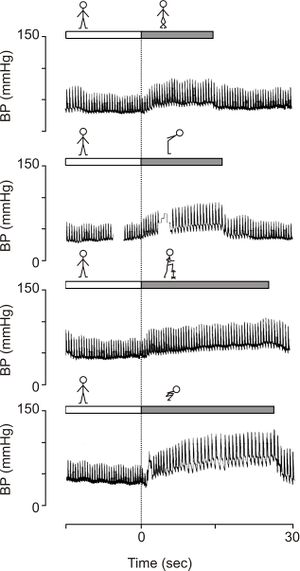
During later visits to our laboratory she was instructed to use other manoeuvres to improve orthostatic tolerance like leg crossing and putting a foot on a chair as demonstrated in Figure 3.
During long-term follow up our patient has been using a combination of these manoeuvres almost automatically i.e. before warning systems occurred in daily life. She never lost consciousness again. However, she still was definitely restricted in her activities and social life activities. Running or doing things in a hurry were avoided. Cycling uphill or against a strong wind were problematic. She went to bed tired and stood up tired. Sleeping with the head elevated every night was mandatory.
In the next few years, 3 children were born. During the pregnancies, she felt extremely well. There were no moments of lightheadedness, she felt less tired and the volume expansion by fludrocortisone was not needed. At age 46 years she had to retire from her job, feeling not only tired, but exhausted by the combination of her demanding job and taking care of a household with 3 children. In this period she experienced chest pain during relative heavy exercises like cycling with a child on the carrier and walking up 2 flights of stairs to the attic. Myocardial ischemia was diagnosed during exercise testing.
After retirement her condition has stabilised. However, her activity level has slowed down considerably. She now uses an electric bike and when she visit the attic she crawl up the 2nd flight of stairs. In a video made about 1 decade after the onset of her illness, the patient describes her own experience. She later made an instruction video for patients was made demonstrating how our patient applied physical counterpressure manoeuvres to increase low standing blood pressures.
Editor's comments
This is a unique case of acute dysautonomia associated with Hodgkin’s disease with almost complete regression of the symptoms of parasympathetic involvement of several organ systems, namely pupillary abnormalities, a dry mouth and disturbed bladder and bowel function after the acute phase. The sympathetic involvement, indicated by incapacitating orthostatic hypotension remained.
During a 30 year follow up the complaints of orthostatic hypotension have been counteracted by volume expansion and the use of physical counterpressure manoeuvres. Details will be dealt with in the Tutorials dealing with countermeasures and chronic volume expansion. Pregnancies in patients with autonomic failure have to the best of our knowledge not been described.
References
-
This case history was published earlier as Wieling W, van Lieshout JJ, van Leeuwen AM. Physical manoeuvers that reduce postural hypotension in autonomic failure. Clin Aut Res 1993; 3: 57-65. We thank Springer Verlag (Darmstadt, Germany) for permitting this reproduction.
- van Lieshout JJ, Wieling W, van Montfrans GA, Settels JJ, Speelman JD, Endert E, and Karemaker JM. Acute dysautonomia associated with Hodgkin's disease. J Neurol Neurosurg Psychiatry. 1986 Jul;49(7):830-2. DOI:10.1136/jnnp.49.7.830 |
- van Lieshout JJ, Wieling W, Wesseling KH, and Karemaker JM. Pitfalls in the assessment of cardiovascular reflexes in patients with sympathetic failure but intact vagal control. Clin Sci (Lond). 1989 May;76(5):523-8. DOI:10.1042/cs0760523 |
- van Lieshout JJ, ten Harkel AD, van Leeuwen AM, and Wieling W. Contrasting effects of acute and chronic volume expansion on orthostatic blood pressure control in a patient with autonomic circulatory failure. Neth J Med. 1991 Aug;39(1-2):72-83.