Disabling orthostatic hypotension caused by sympathectomy performed for hyperhydrosis
Case Report
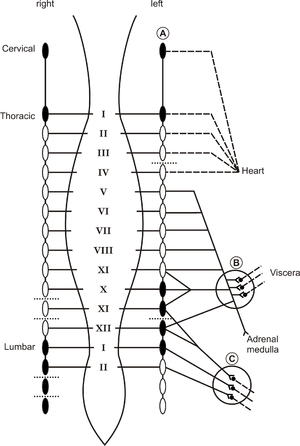
The sites of the lesions in the sympathetic thoraco-lumbar chain are indicated. For clarity the adrenergic innervation of the heart, splanchnic vascular bed and adrenal medulla are shown on the left side only.
..... = interganglionary sympathicotomy
___ = preganglionic fibre
--- = postganglionic fibre
0 = intact sympathetic ganglion
• = ganglionotomy
A = cervical ganglia
B = celiac and superior mesenteric ganglia
C = lower abdominal sympathetic ganglia
An otherwise healthy 38 year-old woman suffered from severe hyperhidrosis of the hands and the feet since childhood, because of which she felt socially withdrawn. Since medical treatment of the hyperhidrosis proved ineffective, she was referred to a clinic for neurovegetative surgery. Extensive sympathectomies were performed over a period of two years, as summarized in Fig. 1. Following thoracoscopic sympathetic ganglionotomies bilaterally at the upper thoracic levels (Th II- Th VI), the excessive sweating of the hands disappeared. In the following year the procedure was extended to the lumbar levels L II - L IV at the left, while interganglionary sympathicotomies at LII - LIV at the right were performed with a salutary effect on plantar hyperhidrosis. After these procedures abnormal sweating developed, located at both dorsal and ventral parts of the trunk. A further right-sided extension of the sympathectomies was performed at the levels Th VII - Th XII, including a re-ganglionotomy at Th VI and an interganglionary sympathicotomy at Th X - Th XII. This resulted in relief of the hyperhidrosis over the right hemi-thorax. Abnormal sweating of the left side of the trunk persisted, while palmar hyperhidrosis returned on the left for which the following procedure was performed on the left side: re-ganglionotomy at Th II - Th V, a ganglionotomy at Th VII - Th IX and an interganglionary sympathicotomy at Th III, IV, XI and XII. Two days before the last procedure she had played a field hockey game in the highest veteran league, indicating an excellent exercise tolerance. Directly following the last operation she complained of dizziness on standing, causing her to become severely disabled preventing her acutely from performing housekeeping duties [1].
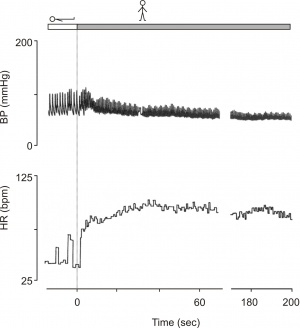
On physical examination at the dorsal thoracic and lumbar regions small scars of the surgical procedures were visible. Neurological examination showed no abnormalities. Supine blood pressure was normal. Upon standing, systolic and diastolic blood pressures dropped markedly (Fig. 2) and dizziness ensued. Heart rate increased from 50 to 85 beats/min in 15 s and to 100 beats/min after 35 s. In spite of the progressive fall in blood pressure heart rate did not increase further but slightly decreased to 95 beats/min after 2 min of standing. Supine values of plasma noradrenaline and adrenaline were abnormally low and there was virtually no increase upon standing.
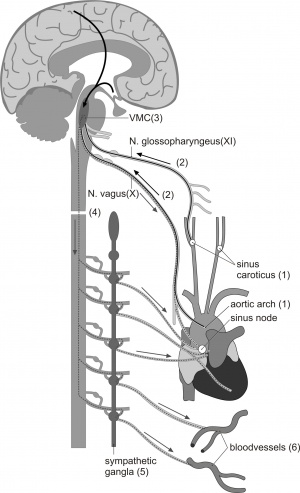
# lesion in the sinus caroticus/aortic baroreceptors # lesion in the sinus caroticus/aortic afferents # lesion in the medulla # spinal cord lesion # preganglionic/ganglionic lesion # postganglionic lesion
Editor's Comment
Hyperhidrosis is a pathological condition of excessive sweating of unknown origin. In patients with hyperhidrosis various non-surgical therapies have been considered. Although anticholinergic drugs seem to be effective, their use has been limited because of side effects [2]. Therefore, in selected cases of hyperhidrosis, destruction of the sympathetic ganglia by thoracoscopic sympathectomy is held as the reference treatment for severe palmar hyperhidrosisis [3]. Notwithstanding thoraco-lumbar sympathectomies cardiovascular control remained sufficient even to meet the needs of prolonged and intermittently vigorous exercise of competitive field hockey. However, after the final surgical procedure that resulted in an almost complete sympathetic denervation of the splanchnic area (Fig 1), symptoms of postural hypotension became manifest. The critical importance of the splanchnic area for the control of blood pressure is well known [4-10]; sympathectomies have little influence on postural blood pressure control until the major part of the sympathetic outflow to the splanchnic area is destroyed [5-7].
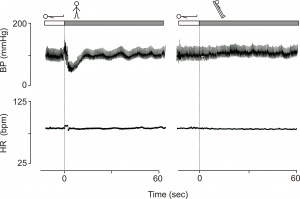
Sympathetic nerve supply to the heart is derived from the segments Th I - Th IV (V), synapsing in all cervical and the upper four (five) thoracic ganglia [2]. In view of the pattern of sympathectomies carried out, therefore, sympathetic innervation of the heart was expected to be at least partially intact (Fig 1) and functional integrity was present upon testing. An abnormally large increase in heart rate (45 bpm) was observed. Thus this patient is a rare example of a hypoadrenergic orthostatic response with intact heart rate control (Fig. 2). The opposite pattern i.e. intact vasomotor control and complete cardiac denervation is observed in patients with a cardiac transplant. In these patients orthostatic blood pressure control is normal despite no increase in heart rate. Figure 3 shows an example of the heart rate and blood pressure response upon active standing and passive head-up tilting in a 38-year-old fit patient with a cardiac transplant.
Patients with circumscribed anatomical lesions on the arterial baroreflex arc provide unique opportunity to study cardiovascular control in otherwise intact humans. Figure 4 provides a schematic drawing of the baroreceptor afferent and autonomic efferent pathways of the baroreflex arc with possible mechanisms of failure of cardiovascular resulting in a tendency to orthostatic hypotension and syncope.