Malignant vasovagal syncope due to blood phobia
N. van Dijk*, S.C.J.M. Velzeboer*, A. Destrée-Vonk§, M. Linzer+ and W. Wieling*
Departments of * Medicine and § Pediatrics, Academic Medical Centre, University of Amsterdam, Amsterdam (The Netherlands), + University of Wisconsin, Madison, Wisconsin (USA)
A 17-year-old boy was referred because of longstanding complaints of fainting. He experienced his first episode at the age of 4 during a venipuncture [1]. Since then he often fainted, first with venipuncture, but later also when he merely thought of blood, needles or other medical procedures. He has no complaints during prolonged standing. His mother experienced the same problem when she was young.
When he was 16 he was evaluated by a pediatrician. When discussing venipuncture, syncope occurred. The patient showed some myoclonic movements and was unconscious for less than five minutes. After regaining consciousness he was pale, sweating and nauseous. Physical examination, ECG and echocardiography showed no abnormalities. On 24 hour Holter monitor recording sinus rhythm, with frequent bouts of sinus arrhythmia ranging from 110 to 58 bpm was observed. During cardiovascular reflex investigation, the patient had a blood pressure of 106/54 mmHg. During deep forced breathing, marked sinus arrhythmia was observed. Standing up elicited a normal blood pressure and heart rate response. The investigators discussed with the patient’s mother the normal results of the tests and mentioned that a “blood taking” provocation might be necessary at another occasion.
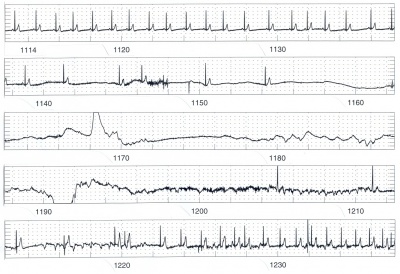
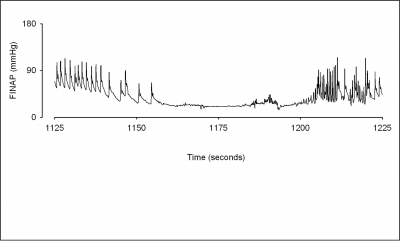
About 1 minute later the patient felt nauseous and started sweating. Bradycardia developed. The patient then became asystolic for almost 50 seconds. He was put on the bed and cardiac massage was applied. When reviewing the ECG afterwards, the first escape beat was almost at the same moment of CPR initiation. After 2 minutes the patient regained consciousness with a normal blood pressure and bradycardia of 45 bpm (Figs. 1 and 2). Syncope due to an emotionally-evoked vasovagal response with extreme bradycardia was diagnosed. Considering the clear cause of fainting and with the patient’s age in mind, we decided not to implant a pacemaker but to refer the patient to the Pediatric Psychosocial Department.
His blood-injury phobia was treated using systematic desensitization with muscle tensing and cognitive techniques [2][3] under surveillance of the pediatric resuscitation team. Cognitive behavioral therapy was used to teach him to apply realistic and reassuring thoughts to the physical symptoms he saw as alarming.
The experience during behavior therapy that straining his muscles immediately diminished negative bodily sensations resulted in effective control over the fear-provoking venipuncture situation. After 10 training-sessions, he was able to undergo venipuncture without fainting. The patient has had no fainting episodes for a follow-up period of 18 months.
Editor's comments
This young patient is unique in 3 ways: First, only thinking of venipuncture was enough to induce a vasovagal response. Secondly, he demonstrated a very long period of asystole (50s) from his blood-phobia-related vasovagal syncope. Thirdly, he was successfully treated using psychological interventions, avoiding the use of a pacemaker.
Vasovagal syncope is a frightening but usually benign condition. A vasovagal collapse can occur after certain triggers (emotional or prolonged standing) which cause a reduction in sympathetic outflow to the systemic circulation and augmentation of efferent vagal activity. In the present case only thinking about blood taking induced an emotional faint. Usually vasodilatation is the most important cause of hypotension in syncope, while bradycardia is often moderate and of late onset.
Treatment with a pacemaker, therefore, has no effect on hypotension in the vast majority of such patients or on the speed with which hypotension occurs [4][5][6]. The asystole clearly was instrumental in causing syncope in this patient. The pronounced sinus arrhythmia during Holter monitoring and forced breathing indicate this patient’s susceptibility to vagal stimulation. Vasovagal syncope with prolonged asystole is uncommon. Deal et al found a cardioinhibitory response (asystole ≥ 5 seconds) in 4.5% of syncopal children during tilt-table testing [7].
Intense fear of seeing blood is seen in 2-4.5% of children and adults. Blood-injury phobia usually starts in childhood, is often familial and is a distinctive focal phobia. Exposure therapy has been described as a valuable method to treat it [8]. In serious cases like this, great care must be taken to motivate patients for treatment, because of their tendency to withdraw from any confrontation with fear-provoking stimuli.
We conclude that vasovagal syncope due to bloodphobia, even with very long periods of asystole, can be treated using psychological techniques instead of pacemaker implantation
References
<biblio>
- VanDijk This case was published earlier as: Van Dijk N, Velzeboer SC, Destree-Vonk A, Linzer M, Wieling W. Psychological treatment of malignant vasovagal syncope due to bloodphobia. Pacing Clin Electrophysiol 2001;24:122-124. . We thank Blackwell Publishing for permitting this reproduction
- Hellstrom pmid=8741718
- Krediet pmid=12270863
- Sra pmid=8455666
- Hainsworth Hainsworth R. Syncope and fainting: classification and pathopsychological basis. In: Bannister R, Mathias CJ, eds. Autonomic failure. A textbook of clinical disorders of the autonomic nervous system. 4th ed. New York: Oxford University Press; 1999:428-36.
- Connolly pmid=12734133
- Deal pmid=9249828
- Marks pmid=3048117
<biblio>